Research & insights
Showing 1-12 results of 279
Community Mental Health Survey 2023 Infographic
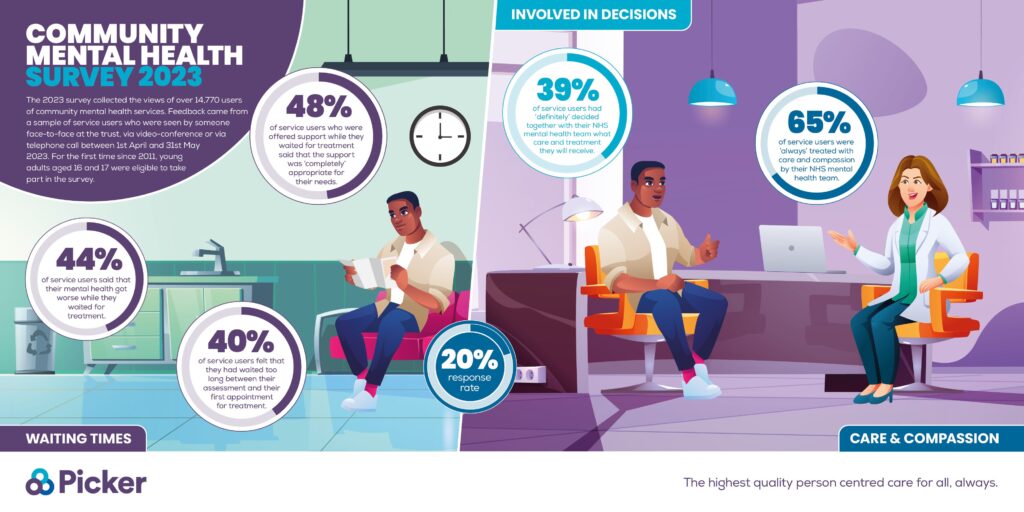
Mental health services struggle to meet demand, according to a major survey

Picker Impact Report 2022/23
Celebrating Patient Experience Week 2024

Picker Group acquires the Patient Experience Network (PEN)

Picker discusses the 2023 NHS Staff Survey Results on HSJ’s Health Check podcast
Infographic of the NHS Staff Survey 2023 headline results

NHS staff experience improving, according to world’s largest workforce survey

Picker’s NHS Manifesto: Our vision for a person centred health service

World Cancer Day: Listening to data to drive person centred cancer care services

2024 Global Patient Survey on Lymphomas & CLL

Picker Chosen by Lymphoma Coalition to Conduct 2024 Global Patient Survey on Lymphomas and CLL

Our principles include